The Endocrine Imbalance
PCOS also means dealing with a complex hormonal storm that not only affects our reproductive health but ripples across our whole body's system. Here’s an in-depth look at how these hormonal disruptions shape our experiences and what we can do to find some balance.
Our Hormonal
Challenges
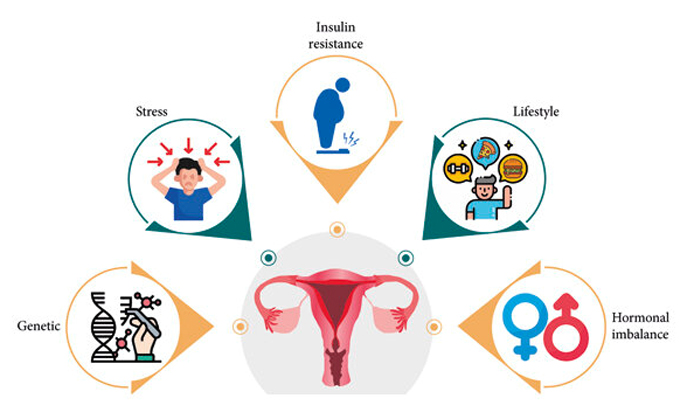
● Rampant Androgens: We
often have higher levels of androgens, like testosterone. This can lead to
those all-too-familiar issues: excess body hair, acne, and thinning hair on our
heads.
● Insulin Struggles: Many of
us face insulin resistance, which means our bodies can't use insulin
efficiently. This results in higher insulin levels that can make our androgen
levels even worse.
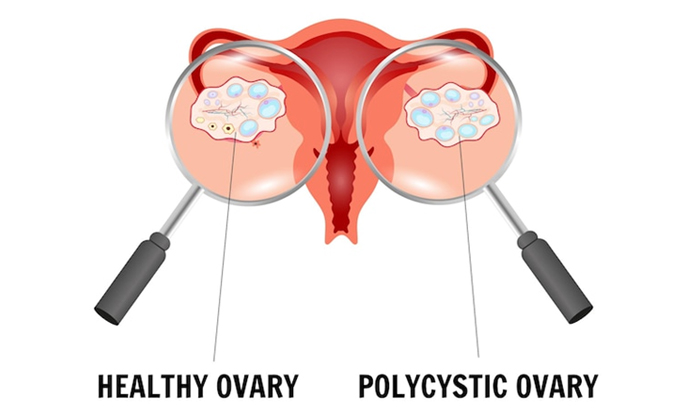
● LH and FSH Imbalance: Our
bodies might produce too much luteinizing hormone (LH) and not enough follicle-stimulating
hormone (FSH). This imbalance can mess up the growth and release of eggs from
our ovaries, leading to missed or irregular periods.
● Low Progesterone: Without regular ovulation, we often don’t produce enough progesterone, which is key for regulating our cycle and supporting pregnancy.
How This Affects
Us?
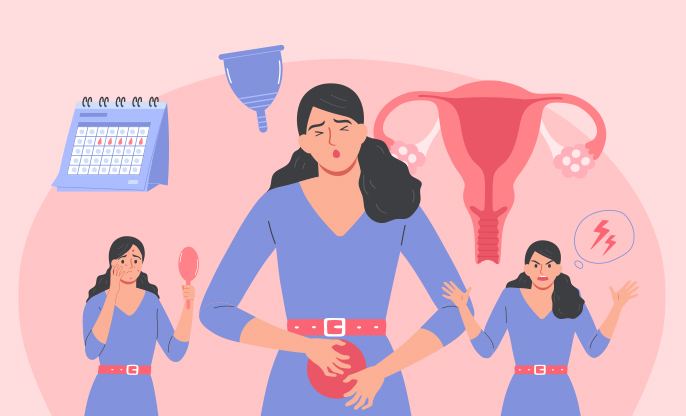
● Menstrual Mayhem: Irregular or
skipped periods are common because our ovulation is so unpredictable.
● Fertility Frustrations:
Difficulty getting pregnant can be heart-wrenching, owing to our less frequent
ovulation.
● Metabolic Concerns: We’re
at a higher risk for things like type 2 diabetes and high cholesterol, thanks
to insulin resistance.
● Emotional Rollercoasters: Hormonal imbalances can also make us more prone to anxiety and depression, which is why our mental health needs as much care as our physical health.
Managing Our
Hormonal Health
● Eating and Moving:
Sticking to a diet low in refined carbs and rich in fiber can boost our insulin
sensitivity. Regular exercise helps too, not just with insulin resistance but
also with managing our weight, which can positively impact our hormonal
balance.
● Medical Options:
○ Metformin: This medication
can help reduce our insulin resistance and lower insulin levels, which may help
with androgen levels too.
○ Birth Control Pills: These
can regularize our periods and lower our androgen levels, which helps with acne
and excess hair.
○ Anti-androgens: Medications
like spironolactone can directly combat the effects of androgens on our skin
and hair.
● Surgical Solutions: Sometimes, procedures like ovarian drilling are suggested to reduce androgen production directly from the ovaries and encourage ovulation.
Living with PCOS is about understanding the delicate interplay of hormones in our bodies and finding ways to restore balance where we can. By adopting a combination of lifestyle changes, medications, and possibly even surgery, we can navigate our symptoms more effectively and embrace a healthier, more balanced life. It's about turning our struggles into strength, one step at a time.